Shoulder Labrum Tears: An Overview - HSS.edu - Hospital for Special Surgery, New York
Dr. Fealy on treatment of labral cartilage tears and shoulder instability
Overview
The labrum is the cup-shaped rim of cartilage that lines and reinforces the ball and socket joint of the shoulder, which is comprised of the glenoid - the shallow shoulder socket - and the head, or ball, of the upper arm bone known as the humerus. The labrum is the attachment site for the ligaments and supports the ball and socket joint along with the rotator cuff tendons and muscles. It contributes to shoulder stability and, when torn, can lead to partial or complete shoulder dislocation.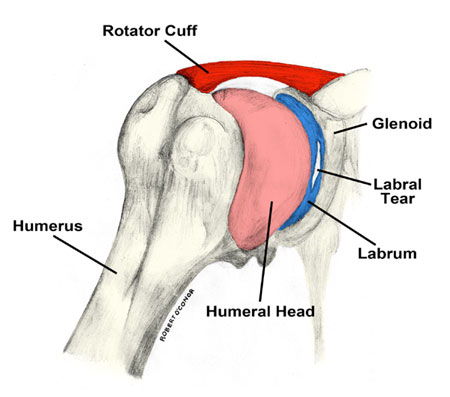
Anatomy of the shoulder, featuring the humerus (upper arm bone) and the labrum,
which rims the glenoid (shoulder socket). [Illustration by Robert O'Conor]
Bankart tears, on the other hand, typically occur with shoulder dislocation in younger patients; the head of the humerus either shifts toward the front of the body, leading to “anterior instability,” or the back of the body, called “posterior instability.”
Both types of tears are usually accompanied by aching pain and difficulty performing normal shoulder movements. With Bankart tears in particular, patients may feel apprehension that the shoulder may slip out of place or dislocate in certain positions. Patients with SLAP tears may experience pain at the front of the shoulder near the biceps tendon.
Unfortunately, labral tears are hard to prevent, especially in athletes, because the force of the overhead motion contributes to the injury. Although athletes are most prone to labral tears, people who experience a traumatic event - such as falling down a flight of stairs - are also at risk, particularly older adults whose cartilage becomes more brittle with age.
Treatment
“Surgeons should try to be as conservative as possible when treating a torn shoulder labrum,” says Dr. Fealy. Surgeons will usually conduct a physical exam and MRI or x-ray, if necessary, to determine the severity of the injury and the treatment needs.SLAP tears are usually treated with rest, anti-inflammatory medications and, in some cases, an in-office cortisone injection. This is followed by gradual stretching of the shoulder, initially with a physical therapist, for six weeks to two months.
If the injury is a minor Bankart tear with a dislocation, the physician (or even the coach or patient themselves) can usually pop the shoulder back into place - a process called reduction - followed by physical therapy to strengthen the muscles.
“If physical therapy fails and the athlete still can’t complete overhead motions, or the shoulder continues to dislocate, surgical treatment might be required to reattach the torn ligaments and labrum to the bone,” says Dr. Fealy. Arthroscopic procedures, in which the doctor operates through a small incision, are usually preferred because they are less invasive than open surgery.
In general, non-surgical treatment is usually most appropriate for older patients who do not engage in regular physical activity, while younger athletes who regularly participate in higher impact sports can expect recurrence and may want to consider arthroscopic surgery.
Prognosis
Patients who undergo arthroscopic repair can expect shorter recovery times and less pain. Those undergoing open surgery should expect more pain, longer recovery, and in some cases incomplete shoulder rotation.Regardless of treatment type, almost all athletes are advised to wear a sling for the first four weeks post-surgery to protect the shoulder as it heals. Following surgery, athletes may require six months to one year for full recovery, with overhead throwing athletes taking the longest.
“If fixed properly, most athletes should be able to return to at least 80 percent of their pre-injury level of play,” says Dr. Fealy.